Another brief tutorial on SI joint dysfunction (from SI-Bone/ifuse implant)
 That most orthopedic tests haven’t been proven definitive in diagnosing some or most musculoskeletal conditions is a given. In fact even those tests with good inter-reliability suffer with short comings in validity. Laslett, Bogduk et al did a systematic review in 2010 to determine whether tests could accurately determine a disc vs. facet vs. an SI joint and found the answer to be “generally NO”. However most experts suggest a barrage of tests (with the majority negative (or positive)) give an acceptable odds-ratio as to the likelihood of involvement. This is more so the case with the SI joint vs. facet or disc.
That most orthopedic tests haven’t been proven definitive in diagnosing some or most musculoskeletal conditions is a given. In fact even those tests with good inter-reliability suffer with short comings in validity. Laslett, Bogduk et al did a systematic review in 2010 to determine whether tests could accurately determine a disc vs. facet vs. an SI joint and found the answer to be “generally NO”. However most experts suggest a barrage of tests (with the majority negative (or positive)) give an acceptable odds-ratio as to the likelihood of involvement. This is more so the case with the SI joint vs. facet or disc.
The above picture from SI-Bone suggests a clinical testing procedure with the (5) most diagnostically-relevant SI tests. IF (4) of the (5) are positive there is a 75% likelihood the SI may be involved. The opposite is true as well ((4) of (5) negative). However other studies suggest the MOST relevant tests are the THIGH TRUST and distraction/compression. These (2) tests tended to give the strongest indications.

 When designing the Kdt Neural-flex it was decided NO cumbersome split-bolster, dual rubber bolsters or ridiculous support-stool would be used. Instead we created a revolutionary configuration incorporating leg-support and attendant pelvic ‘flattening’ into the table…eliminating the need for bolsters. In our testing clinics and now in the field for nearly 8 years this has proven itself to be a very important table attribute. (1); CA’s and doctors don’t need to wrestle the bolsters under the knees before and after every session…and store them when not in use. (2); proper placement, which was always an annoying is no longer a consideration, as is their shifting around and getting the belt caught under one or the other. (3); the patient isn’t required to activate the hip-flexors before or after the treatment to move the bolsters under the legs. The knees stay bent and the table section meets them. Those of us who’ve spent years monkeying with bolsters (and I should know since I designed and developed the DTS dual-bolsters and had to use them for years) the incorporation into the table was nothing short of incredible. The small ½ round bolster can enhance comfort in some patients either placed under the ankles or under the crook of the knee. With the pelvis “affixed” to the table via the flexed-section under the legs a greater participation and control of the traction is assured.
When designing the Kdt Neural-flex it was decided NO cumbersome split-bolster, dual rubber bolsters or ridiculous support-stool would be used. Instead we created a revolutionary configuration incorporating leg-support and attendant pelvic ‘flattening’ into the table…eliminating the need for bolsters. In our testing clinics and now in the field for nearly 8 years this has proven itself to be a very important table attribute. (1); CA’s and doctors don’t need to wrestle the bolsters under the knees before and after every session…and store them when not in use. (2); proper placement, which was always an annoying is no longer a consideration, as is their shifting around and getting the belt caught under one or the other. (3); the patient isn’t required to activate the hip-flexors before or after the treatment to move the bolsters under the legs. The knees stay bent and the table section meets them. Those of us who’ve spent years monkeying with bolsters (and I should know since I designed and developed the DTS dual-bolsters and had to use them for years) the incorporation into the table was nothing short of incredible. The small ½ round bolster can enhance comfort in some patients either placed under the ankles or under the crook of the knee. With the pelvis “affixed” to the table via the flexed-section under the legs a greater participation and control of the traction is assured.

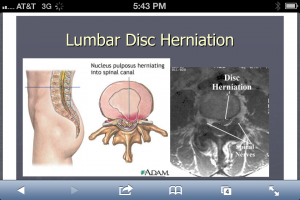 Not that we haven’t all seen these pictures innumerable times but it is wise to recognize both the classic look on MRI and the illustration. It’s also important to recognize these presentations are neither ubiquitous nor inherently ominous if you look at population studies. Lifetime prevalence of a “true pinched nerve” is about 10% and both old and recent studies show self-healing, resolution is very common…if not ubiquitous. Many studies conclude there is shrinkage-phenomena i.e. up to 80% of hernias will shrink at least 50% in 6-9 months. And those patients presenting with HNP (typically a younger population) actually recovered with better outcomes than those having similar pain but no MRI confirmed herniation, in 6-9 months (NEJM 10.1056).
Not that we haven’t all seen these pictures innumerable times but it is wise to recognize both the classic look on MRI and the illustration. It’s also important to recognize these presentations are neither ubiquitous nor inherently ominous if you look at population studies. Lifetime prevalence of a “true pinched nerve” is about 10% and both old and recent studies show self-healing, resolution is very common…if not ubiquitous. Many studies conclude there is shrinkage-phenomena i.e. up to 80% of hernias will shrink at least 50% in 6-9 months. And those patients presenting with HNP (typically a younger population) actually recovered with better outcomes than those having similar pain but no MRI confirmed herniation, in 6-9 months (NEJM 10.1056). We designed the articulations of the Neural-flex so a modest ‘Inversion’ position could be achieved by simply pressing two buttons simultaneously on the controller. The inversion posture allows approx. 35° of declination either prone or supine. The Prone-declined position creates a robust ‘unique selling proposition’ especially with the addition of various instrument adjusting procedure (such as Arthro-Stim or similar units). Utilizing the overt muscular-relaxation from the declination adds the selling-proposition that a better adjustment results due to lessened postural muscular ‘activity’. Additionally massage and manipulation are both clinically enhanced with inversion for similar reasons. We suggest 3-4 total minutes of massage (manual or mechanical) then a return to neutral for 10-30 seconds, then repeat. We’ve found good results and excellent patient receptivity to this procedure. Manual distraction (thumbs or thenar) is also easily added as the proximal table section remains unlocked allowing it to slide forward increasing the sense of lumbar and thoracic ‘stretch’. In this position it’s also interesting to try reflexology/foot massage or foot/ankle manipulation.
We designed the articulations of the Neural-flex so a modest ‘Inversion’ position could be achieved by simply pressing two buttons simultaneously on the controller. The inversion posture allows approx. 35° of declination either prone or supine. The Prone-declined position creates a robust ‘unique selling proposition’ especially with the addition of various instrument adjusting procedure (such as Arthro-Stim or similar units). Utilizing the overt muscular-relaxation from the declination adds the selling-proposition that a better adjustment results due to lessened postural muscular ‘activity’. Additionally massage and manipulation are both clinically enhanced with inversion for similar reasons. We suggest 3-4 total minutes of massage (manual or mechanical) then a return to neutral for 10-30 seconds, then repeat. We’ve found good results and excellent patient receptivity to this procedure. Manual distraction (thumbs or thenar) is also easily added as the proximal table section remains unlocked allowing it to slide forward increasing the sense of lumbar and thoracic ‘stretch’. In this position it’s also interesting to try reflexology/foot massage or foot/ankle manipulation.