Decompression Force Calculus
In a general sense there can be no absolutely accurate ‘traction-force calculation’ since most mechanical attributes patient to patient are unknown. However we have to make assumptions and these are based on both morphology, function, patient condition and duration of pain. It makes sense to “limit the liability” in ALL cases, however limiting the pull force (tension) in ALL cases could let patients needing robust, high-force procedures to slip through “underserved”. The more ‘Acute’ the condition the lighter the pull. Acute both in temporal-terms and level/intensity of pain. Since most moderate or severe LBP (or neck pain) is indubitably a SPRAIN or annular compromise overstretching it early on is utterly counterproductive. The VAX-D protocol called for a 3-4 week “cooling off” period where “real/traction-able/traction-responsive” conditions were allowed to simmer…becoming more apparent after several weeks of natural de-inflammation/healing. After which, persistent symptoms gave a green light to decompression. The more chronic the symptom the more relavant higher force MAY be…but as discussed before; degenerative disc fibers are not infinetly adaptable to stretch, and can sustain injury if overloaded. And that could mean prolapse in the worse scenario.
We seem to agree 30-35% TBW is a good starting point for sub-acute/chronic conditions whose symptoms are LB with or without some pelvic/thigh referral. Sub-acute is typically likely at least 2-3 weeks since onset. Acute presentations (you feel compeled to decompress) its best to stick to 20-30% TBW with a TRAC-short pull (10-15 secs pull/rest, 5-8 min). IF it’s a compromised condition you probably will not have crippled them too badly.
I routinely say: “don’t be dogmatic about high force OR low force”, our rules are guide posts. There are many patients (yes typically big men) who do require (or demand) serious force (90-120 pounds) however more patients require less force and are better served at 30-35%.

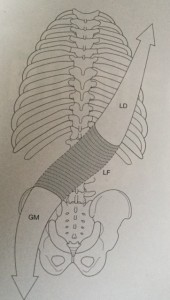
 When designing the Kdt Neural-flex it was decided NO cumbersome split-bolster, dual rubber bolsters or ridiculous support-stool would be used. Instead we created a revolutionary configuration incorporating leg-support and attendant pelvic ‘flattening’ into the table…eliminating the need for bolsters. In our testing clinics and now in the field for nearly 8 years this has proven itself to be a very important table attribute. (1); CA’s and doctors don’t need to wrestle the bolsters under the knees before and after every session…and store them when not in use. (2); proper placement, which was always an annoying is no longer a consideration, as is their shifting around and getting the belt caught under one or the other. (3); the patient isn’t required to activate the hip-flexors before or after the treatment to move the bolsters under the legs. The knees stay bent and the table section meets them. Those of us who’ve spent years monkeying with bolsters (and I should know since I designed and developed the DTS dual-bolsters and had to use them for years) the incorporation into the table was nothing short of incredible. The small ½ round bolster can enhance comfort in some patients either placed under the ankles or under the crook of the knee. With the pelvis “affixed” to the table via the flexed-section under the legs a greater participation and control of the traction is assured.
When designing the Kdt Neural-flex it was decided NO cumbersome split-bolster, dual rubber bolsters or ridiculous support-stool would be used. Instead we created a revolutionary configuration incorporating leg-support and attendant pelvic ‘flattening’ into the table…eliminating the need for bolsters. In our testing clinics and now in the field for nearly 8 years this has proven itself to be a very important table attribute. (1); CA’s and doctors don’t need to wrestle the bolsters under the knees before and after every session…and store them when not in use. (2); proper placement, which was always an annoying is no longer a consideration, as is their shifting around and getting the belt caught under one or the other. (3); the patient isn’t required to activate the hip-flexors before or after the treatment to move the bolsters under the legs. The knees stay bent and the table section meets them. Those of us who’ve spent years monkeying with bolsters (and I should know since I designed and developed the DTS dual-bolsters and had to use them for years) the incorporation into the table was nothing short of incredible. The small ½ round bolster can enhance comfort in some patients either placed under the ankles or under the crook of the knee. With the pelvis “affixed” to the table via the flexed-section under the legs a greater participation and control of the traction is assured.

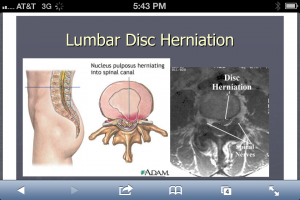 Not that we haven’t all seen these pictures innumerable times but it is wise to recognize both the classic look on MRI and the illustration. It’s also important to recognize these presentations are neither ubiquitous nor inherently ominous if you look at population studies. Lifetime prevalence of a “true pinched nerve” is about 10% and both old and recent studies show self-healing, resolution is very common…if not ubiquitous. Many studies conclude there is shrinkage-phenomena i.e. up to 80% of hernias will shrink at least 50% in 6-9 months. And those patients presenting with HNP (typically a younger population) actually recovered with better outcomes than those having similar pain but no MRI confirmed herniation, in 6-9 months (NEJM 10.1056).
Not that we haven’t all seen these pictures innumerable times but it is wise to recognize both the classic look on MRI and the illustration. It’s also important to recognize these presentations are neither ubiquitous nor inherently ominous if you look at population studies. Lifetime prevalence of a “true pinched nerve” is about 10% and both old and recent studies show self-healing, resolution is very common…if not ubiquitous. Many studies conclude there is shrinkage-phenomena i.e. up to 80% of hernias will shrink at least 50% in 6-9 months. And those patients presenting with HNP (typically a younger population) actually recovered with better outcomes than those having similar pain but no MRI confirmed herniation, in 6-9 months (NEJM 10.1056). We designed the articulations of the Neural-flex so a modest ‘Inversion’ position could be achieved by simply pressing two buttons simultaneously on the controller. The inversion posture allows approx. 35° of declination either prone or supine. The Prone-declined position creates a robust ‘unique selling proposition’ especially with the addition of various instrument adjusting procedure (such as Arthro-Stim or similar units). Utilizing the overt muscular-relaxation from the declination adds the selling-proposition that a better adjustment results due to lessened postural muscular ‘activity’. Additionally massage and manipulation are both clinically enhanced with inversion for similar reasons. We suggest 3-4 total minutes of massage (manual or mechanical) then a return to neutral for 10-30 seconds, then repeat. We’ve found good results and excellent patient receptivity to this procedure. Manual distraction (thumbs or thenar) is also easily added as the proximal table section remains unlocked allowing it to slide forward increasing the sense of lumbar and thoracic ‘stretch’. In this position it’s also interesting to try reflexology/foot massage or foot/ankle manipulation.
We designed the articulations of the Neural-flex so a modest ‘Inversion’ position could be achieved by simply pressing two buttons simultaneously on the controller. The inversion posture allows approx. 35° of declination either prone or supine. The Prone-declined position creates a robust ‘unique selling proposition’ especially with the addition of various instrument adjusting procedure (such as Arthro-Stim or similar units). Utilizing the overt muscular-relaxation from the declination adds the selling-proposition that a better adjustment results due to lessened postural muscular ‘activity’. Additionally massage and manipulation are both clinically enhanced with inversion for similar reasons. We suggest 3-4 total minutes of massage (manual or mechanical) then a return to neutral for 10-30 seconds, then repeat. We’ve found good results and excellent patient receptivity to this procedure. Manual distraction (thumbs or thenar) is also easily added as the proximal table section remains unlocked allowing it to slide forward increasing the sense of lumbar and thoracic ‘stretch’. In this position it’s also interesting to try reflexology/foot massage or foot/ankle manipulation.