Compression demands ‘decompression’….
After a decade in practice I began to think ‘disc’ problems were not responding as I would hope they would. This concern is a major one since a vast majority of our most motivated and disconcerted patients are dealing with a disc hernia or other disc issue. I began to investigate the VAX-D and the concept of decompression and I was sold. Twenty year later I may have altered my level of skepticism toward ‘magic decompression machines’ but not toward the potency of traction-based therapies and the amazing “sell-ability” and relevance to patient retention.
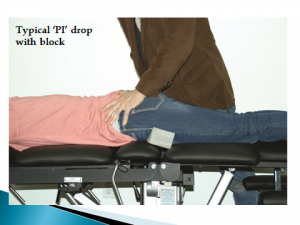
A compression issue simply ‘demands’ a ‘decompression’ treatment solution. Intuitive and logical assessment never guarantees a great outcome but it sure is a lot easier to sell and relate than an ‘irrelevant’ procedure. IF a patient feels better lying down ‘decompression’ is NEVER an inappropriate treatment. That a patient already tends to understand this cannot be over emphasized. The ROF’s must make clear the interconnection and natural benefit decompression will create…BUT that it takes time, commitment and a multi-focal approach. It is in allied treatments where “sell-ability” and strong closing makes its’ mark. Our Kdt table features, “open” belt and pertinent classification are designed to focus patient-problems TO table-solutions.
Table vibration (supine), bolster-less leg/pelvic support & tilt, extension-at-the-waist (prone) and Laser DURING decompression are just such propositions. These attributes and treatment propositions are still very unique in the marketplace and allow excellent compelling clinical selling points.

 Many of those who attend our certification seminars are
Many of those who attend our certification seminars are